Moving Forward with Parkinson’s Disease
Deep brain stimulation (DBS) gives retired physician improved mobility, quality of life
When Martin Adler lost his sense of smell in his mid-50s, he first thought it was due to a sinus surgery. He then started having problems sleeping and difficulty concentrating. When he jogged, his left arm didn’t swing like it normally would.
During the next few years, new symptoms continued to appear. Martin began to feel extreme fatigue, putting an end to his 11-hour work days as an internal medicine and endocrinology physician. He had trouble with fine motor coordination, and developed nerve pain in his lower spine.
Martin, now 69 and retired, had been a physician for 30 years.
“I thought I was a pretty good diagnostician,” he says. “But I didn’t recognize my own symptoms.”
It all came together in November 2003, the evening before Martin’s 57th birthday.
“It was the end of a long day, and I was standing in the hallway,” he recalls. “And this expert neurologist I’d known for years walked by and said to me point blank, ‘You have Parkinson’s disease.’ Now maybe that wasn’t the best approach, but I realized he was absolutely right.”
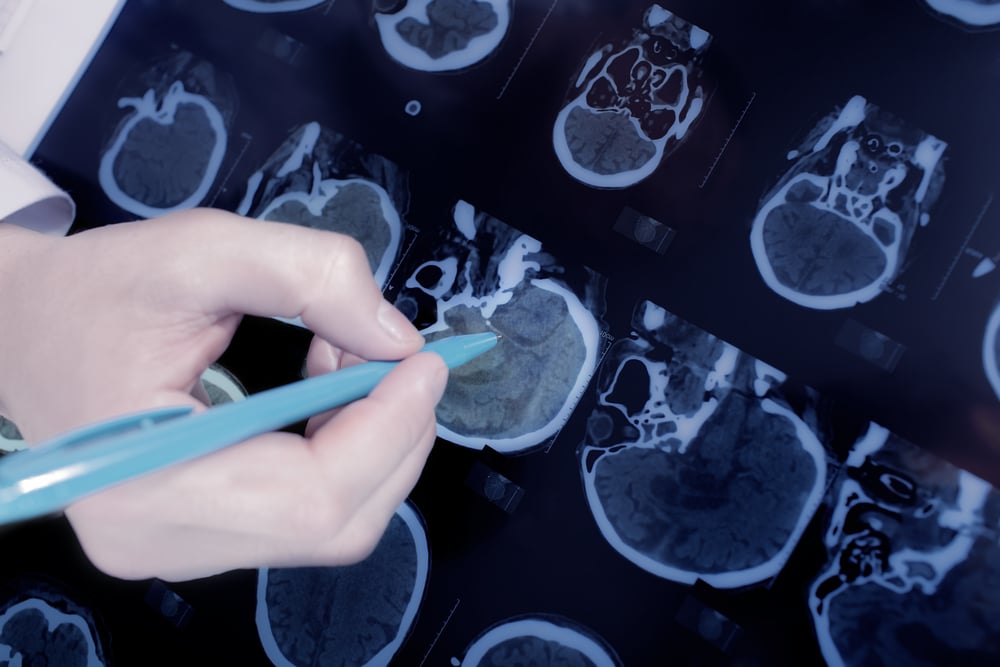
Parkinson’s disease is a progressive, neurodegenerative brain disorder that occurs when the brain cells that produce dopamine, a neurotransmitter that helps control muscle movement and coordination, are damaged or impaired. Symptoms may be mild at first, but may become more significant as the disease progresses. Common symptoms include tremor or shaking of the face or extremities, stiffness, involuntary movements, balance problems, and difficulty walking or speaking. In severe cases, symptoms can become debilitating.
Watch Martin’s story
The DBS treatment journey begins
After the shock wore off, Martin focused on what to do next. He had undergone heart surgery at Scripps in the past, and trusted Scripps for his care. He began seeing Melissa Houser, MD, a neurologist, fellowship-trained movement disorder specialist and medical director of the Shiley Brain Research Center and the Cowling Movement Disorder Clinic at Scripps Clinic.
He started taking the medication levodopa to control his symptoms, but over the next several years, it became progressively less effective and he had to take it more frequently. Martin went from taking levodopa every five hours to every 90 minutes, and he began having unpleasant side effects.
“I felt like I was in quicksand, literally stuck,” he says. “I was having trouble with the general activities of daily living. It would take 10 or 15 minutes just to put my belt through the loops.”
Several years earlier, Dr. Houser had mentioned that Martin could be a candidate for a treatment known as deep brain stimulation (DBS). By delivering electrical stimulation to targeted areas of the brain, DBS overrides the abnormal signals that cause Parkinson’s symptoms and help to restore normal movement.
During DBS surgery, the neurosurgeon places a thin lead, each with four electrodes at the end, in each hemisphere of the patient’s brain. The electrodes are connected to an impulse generator, similar to a pacemaker, which is implanted in the chest. The generator emits a mild current that disrupts abnormal brain signals to reduce or even eliminate symptoms; the current can be adjusted to change the stimulation without additional surgery. It can be shut off at any time, and the entire procedure is completely reversible.
The innovative surgical procedure has been found to greatly reduce the severity of Parkinson’s symptoms, especially in patients who have previously responded to medication.
“In the properly selected patient it can control all cardinal symptoms of Parkinson’s disease — tremor, stiffness, slowness, movement,” says Dr. Houser. “When patients enter this team process, it is a highly individualized evaluation specifically tailored for each patient. They will see several clinicians, a nurse practitioner, a neuropsychologist, a movement disorder specialist, neurosurgeon, speech therapist and physical therapist. Then we can tailor the exact pacer we want to put in their brain and where we want to put it to make sure the patient has the best procedure they can possibly get.”
In August 2014, Scripps Clinic neurosurgeon Adam Burdick, MD, placed the electrodes only in the right side of Martin’s brain, since the majority of his symptoms affected the left side of his body. Two weeks later, Dr. Burdick implanted the generator under Marty’s collarbone and connected the wires to the electrodes.
Immediate improvement in Parkinson’s symptoms
Almost right away, Martin began to notice a tremendous improvement. For several weeks after the surgery, nurse practitioner Sherrie Gould, MSN, who works with Dr. Houser, continued to fine-tune the generator to get the most benefits with the least side effects. He now sees Sherrie monthly.
“It worked very well. I’m faster, I’m not as stiff and my speech is stronger. I bicycle 10 miles every Friday. I go to the gym and do Tai Chi and resistance exercises,” he says. “I was able to get my medication down from 1,000 mg of levodopa to 550 mg.”
Deep brain stimulation has also helped Martin’s wife Eileen.
“This is such a benefit to any care partners, because patients can do so much more for themselves,” adds Martin. “I’m a guy who cherishes his independence and I wanted to be able to drive and take care of my own needs. I would do it again in an instant. It gives me time because treatments will continue to get better.”

Join our Senior Wellness Society for the latest news on Medicare and tips for healthy living in San Diego!
Sign up now ›Are you looking for specialized medical care in San Diego?
Our directory has more than 850 doctors in San Diego County of various specialties who are available to help you.
Find a doctor